SMILE™误入下层对手术时间和视觉结果的影响
通讯作者:周行涛
通讯单位:复旦大学附属眼耳鼻喉科医院
发表杂志:BMC Ophthalmol.
Zheng K, Han Y, Wang J, Han T, Zhou X. Impact of unintended initial dissection of the posterior plane during SMILE surgery on surgery time and visual outcomes. BMC Ophthalmol. 2022 Mar 8;22(1):108. doi:10.1186/s12886-022-02333-x. PMID: 35260116.
背景:
SMILE™凭借其无瓣、微创、保护角膜生物力学的优势,使其成为一种全球流行的角膜屈光手术术式。但是,该手术不同于制瓣手术,需要通过2-4mm角膜小切口来对角膜内透镜进行上下层分离,再取出透镜,故SMILE™的学习曲线相对更长,而术中对透镜上下层的识别非常重要,本研究探讨了误入下层并分离对SMILE™手术时长和术后效果的影响,为误入下层后的治疗效果提供了宝贵的循证医学证据。
摘 要
目的
研究SMILE™术中误入下层分离(UIDPP)后对手术时间和术后视觉结果的影响。
设计
回顾性研究。
方法
基于分析手术录像中有无出现误入下层分离信号,将术眼分为常规组和误入下层分离(UIDPP)组。同时,根据误入下层后是否完全分离透镜后表面,将UIDPP组进一步分为早期察觉和晚期察觉组,分析患者人口学特征、术前检查数据、手术时长及术后结果。
结果

UIDPP: 误入下层分离;IQR: 四分位数范围;UCVA: 裸眼视力
▲正常组和UIDPP组患者术后参数对比

*p<0.05: 与常规组对比;#p<0.05: 与早期察觉组对比;IQR: 四分位数范围;UCVA: 裸眼视力
▲正常组、早期察觉组和晚期察觉组术后参数对比

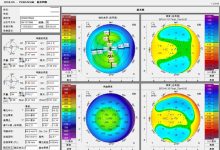
A: 术前最佳矫正视力和术后1天裸眼视力对比累积直方图;B: 术前最佳矫正视力和术后1年裸眼视力对比累积直方图;C: 术后1年等效球镜分布图;D: 术后1年最佳矫正视力的改变;E: 术后1年等效球镜可预测性;F: 术后1年屈光稳定性
▲UIDPP组术后1天和1年的随访数据
研究纳入66名患者(66眼),其中UIDPP组24眼(早期察觉组13眼,晚期察觉组11眼)。UIDPP组比常规组有更小的光学区(中位数6.5 vs 6.6,p=0.007)和更长的手术时间(中位数189.5 vs 91.0,p<0.001)。早期察觉组的手术时间明显小于晚期察觉组(中位数 139.0 vs 489.0,p<0.05),同样常规组的手术时间也小于晚期察觉组(中位数 91.0 vs 489.0,p<0.05),但是光学区的差异仅存在于晚期察觉组和常规组中(中位数 6.5 vs 6.6,p<0.05)。在一年的随访期间,裸眼视力大于等于20/20的眼占87.5%,等效球镜与目标屈光度差异控制在±0.50 D以内的眼占75%,1年内只有1眼下降了1行Snellen视力。
结论
SMILE™中误入下层分离的发生会明显延长手术时间,但并未对患者术后的远期视力造成影响。尽早识别误入下层的信号有助于减少手术时间。
SMILE™手术通常要求先进行透镜上层分离,再进行透镜下层分离,而无论上下层的分离顺序与否,正确识别透镜的上下层,以及及时发现错层的信号都非常重要。虽然本文研究显示误入下层分离后仅延长了手术时间,并未对患者的远期视力造成影响,但这都建立在及时发现错层并正确分离的前提下。若未能及时发现错层,在延长手术时间的同时,可能会出现术后的角膜帽皱褶,角膜水肿,透镜撕裂,甚至角膜假道或穿孔等,故错层分离对患者的术后视力具有潜在的威胁。
Impact of unintended initial dissection of the posterior plane during SMILE surgery on surgery time and visual outcomes
Ke Zheng , Yinan Han , Jing Wang , Tian Han , Xingtao Zhou
Abstract
PURPOSE
To study the impact of unintended initial dissection of the posterior plane (UIDPP) on operation time and surgical outcomes during small incision lenticule extraction (SMILE) surgery.
SETTING
Ophthalmology Department, Eye & ENT Hospital, Fudan University.
METHODS
This was a retrospective study. Based on the SMILE procedure video, the operating eyes were assigned to the normal and UIDPP groups according to the presence or absence of UIDPP signals during surgery. The UIDPP group was further separated into early and late detection based on whether the complete dissection of the lenticule posterior plane or not. Patient's demographic data, preoperative evaluation data, operation time and postoperative outcomes were collected.
RESULTS
Sixty-six patients (66 eyes) who underwent SMILE were included, with 24 eyes with UIDPP (13 in the early detection group and 11 in the late group). The optical zone was smaller (median 6.5 vs. 6.6, P = 0.007), and the operation time was longer (median, 189.5 vs. 91.0 s, P < 0.001) in the UIDPP group compared with normal group. There were significant differences in operation time between the late detection group and early detection group (median, 489.0 vs. 139.0 s, P < 0.05) and between the late detection group and normal group (median 489.0 vs. 91.0 s, P < 0.05), while the optical zone was different only between the late detection and normal groups (median, 6.5 vs. 6.6, P < 0.05). At the one-year follow-up, UDVA was better than or equal to 20/20 in 87.5% of eyes, and 75% of eyes were within ± 0.5 D of the intended refractive target. One eye lost one Snellen line.
CONCLUSIONS
The occurrence of UIDPP will significantly prolong the operation time, but not affect the recovery of long-term visual acuity after surgery. Detecting UIDPP earlier could help shorten the operation time.
本篇文章来源于微信公众号: SMILE屈光天地













 全飞秒
全飞秒 半飞秒
半飞秒 圆锥角膜
圆锥角膜 学术速递
学术速递

